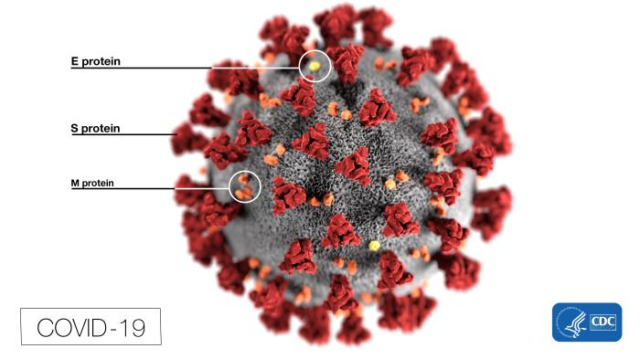
Proteins jutting out from the virus bind to angiotensin-converting enzyme 2 (ACE2) in the alveoli. ACE2 receptors are also found in the linings of blood vessels and airways.
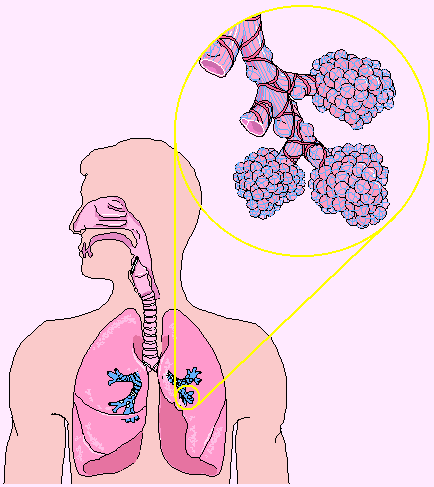
It appears that ACE2 receptors in alveoli deep in the lungs are where the COVID-19 coronavirus likes to bind and replicate. The physics of lung deposition mean that the virus has to be respirable – less than 10 microns or 10/1000 mm to even get to the lungs. Only droplets less than 0.5 microns containing the tiny (0.05 microns) COVID-19 viruses can penetrate deep into the lungs to the alveoli.
This means that whatever the face-mask used, its seal to the face is critical.

The following factors are important:
- When you exhale, air flows in long plumes. When you inhale it is not directional and tends to flow over the surface of the face. A face mask adds resistance to flow, so more tries to flow through breaks in the seal. A small gap of 1mm is 1,000 microns, massive compared to a 0.5 microns droplet that ends up in the alveoli.
- Surgical masks are designed to catch droplets in exhaled air. They cannot stop small droplets entering the lungs through the poor seal when you inhale. They are designed to protect patients from care givers, not to protect the wearer.
- Only COVID-19 containing droplets much less than 10 microns are really important to infections. Only droplets less than 10 microns get deep into the lungs and only droplets less than about 0.5 microns get to the alveoli.
This video published by the US Department of Labor explains the difference between Surgical Masks and Respirators. In Australia P2 face masks are equivalent to N95 masks.
